Vestibular Rehabilitation (Dizziness and Vertigo)
Dizziness is not necessarily vertigo!
Have you ever experienced dizziness and the Doctor tells you it is vertigo? Yet you are not responding to the vertigo treatment? There is a chance that the symptoms are not from a classic BPPV (benign positional paroxysmal vertigo) because there are many other reasons why you could feel dizzy.
There are other vestibular sources that can provide dizziness and to understand where it is from, you need to know more about the vestibular system.
Anatomy
In your body there are 3 systems to keep you in balance:
- Eyes/vision
- Vestibular system
- Proprioceptive system
These 3 systems work together, so if one of them is lacking you might suffer from dizziness as a symptom. For example, if you have glasses and a stiff neck because of anxiety, your vestibular system has to work harder to compensate for the two others. If the 3 systems are not coordinated it might result in vestibular problem.
Cervicogenic dizziness is a diagnosis of exclusion. This means that when the medical and vestibular problems are ruled out you can consider this diagnosis.
The main characteristics of this problem are feeling imbalance and having neck dysfunction or pain.
Symptoms
Many people are surprised to know that their symptoms could come from their neck. Cervicogenic dizziness can provide symptoms such as faintness, disorientation, imbalance and perception of spinning (inside vertigo). Along with those symptoms you will have a lack of cervical spine range of motion (ROM) and probably pain. The dizziness can last from minutes to hours, compared to BPPV (seconds).
Causes
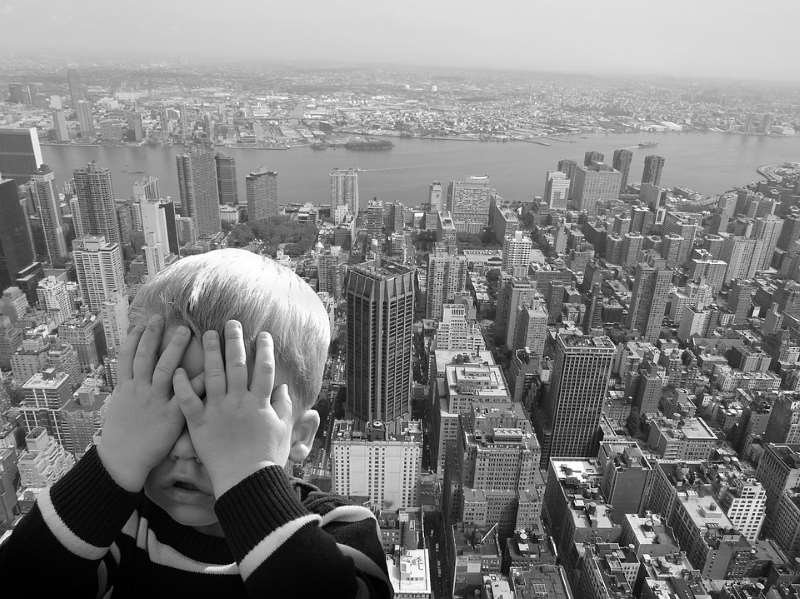
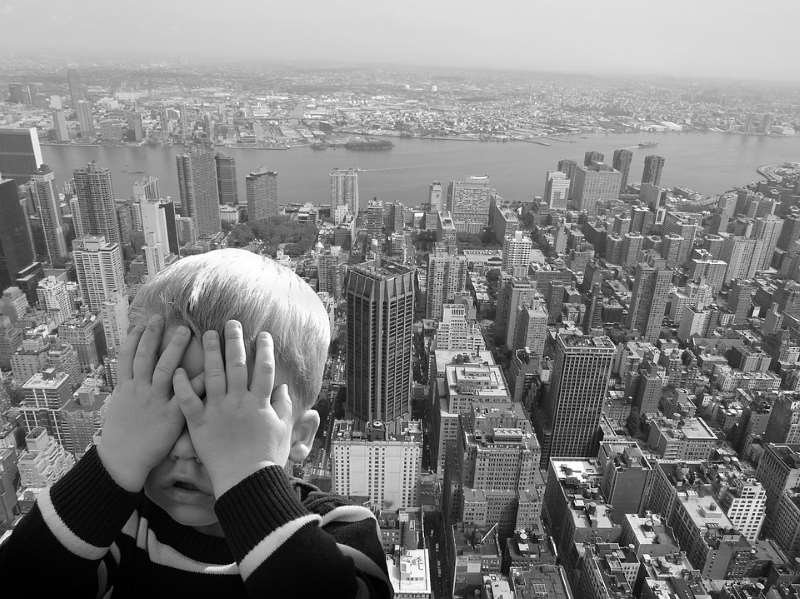
Studies put forward explanations to those symptoms and the first possible cause they agree on for cervicogenic dizziness would be a physical injury and/or psychological issues. For example, a physical injury could be falling, a whiplash or a head concussion. The psychological issues could be depression/anxiety, employment difficulties, fear of space etc. It is good to mention that you can find in some people cervicogenic dizziness combined with any other vestibular problem. For instance, people with BPPV could still feel dizzy even after getting rid of their vertigo.
To conclude, cervicogenic dizziness is all about the input (information) brought to the vestibular nuclei. With 6x more receptors in the neck versus the rest of the body, the information from the cervical spine to the head (here vestibular system and vision) is really important to feel balanced.
Now, how can we treat cervicogenic dizziness?
Some studies say that manual therapy has good result with this kind of problem. Usually when the neck ROM is restored and pain has gone, the dizziness symptoms will go away too. That combined with vestibular exercises can provide the patient with long term improvement. It is important to have a good assessment of the problem in physiotherapy to make sure the right diagnosis is identified. Some physical therapists are qualified in differentiating between the many vestibular problems. A neck assessment should be done in addition of the temporomandibular joint and cranial area if necessary.
Sources:
- Yaseen, K. and al., The Journal of Physical Therapy Science, Vol. 30, No. 1, 2018
- Reiley, A. and al., Archives of Physiotherapy (2017) 7:12
- Wrisley, D. and al., Journal of Orthopaedic and Sports Physical Therapy, Vol. 30, No. 12, December 2000

Vestibular Rehabilitation (Dizziness and Vertigo)
While many people consider seeing a physiotherapist to help with their recovery after an injury or surgery, few consider scheduling a physiotherapy appointment for injury prevention. When it comes to fall prevention, we observe and assess functional movements including your walking pattern, balance and lower extremity strength. A personalized program including education and home exercises can then be designed based on the information we gather from the assessment to help improve your strength, balance and walking pattern.
To avoid tripping while walking, it is important to develop a safe walking pattern. The swing through leg should be lifted high enough to properly clear the ground. A shuffle pattern can result in catching the toe and tripping. Also, since a large portion of walking is spent standing on one foot while the other leg is swinging through, we want to assess balance and stability on the stance leg. If unsteadiness is noted while standing on one foot, a walking aid such as a cane or walker can be beneficial to add stability and support. A physiotherapist can adjust a walking aid and provide instructions and a demonstration. A physiotherapist can also teach safe and effective exercises to help improve walking pattern and endurance for those who feel weak or unsteady while walking.
It is very important to stay active and keep moving. Daily physical activity is essential to maintain aerobic endurance, lower extremity strength and balance. It is never too late to start an exercise program. It is best to think of exercise as a slow gradual progression rather than an all or none activity. It is important that you find an activity that is enjoyable to you to stay motivated and keep active. This may include walking, hiking, cycling, swimming, tennis or golfing. In addition to aerobic activity, a physiotherapist can design an appropriate home exercise program to help improve endurance, balance, coordination and strength.

Vestibular Rehabilitation (Dizziness and Vertigo)
An area of concern that I often hear about while working with an older population is the fear of falling. It is also fairly common that I will assess and treat an injury that is the result of a fall. A fall may occur due to poor balance, an unsafe walking pattern or general deconditioning.
Many older people tell me that they simply avoid physical activity due to the fear of falling and the risk of an injury. The problem with this approach is that as we become less active we experience a gradual decline in muscle strength, endurance, flexibility and balance. This gradual deconditioning puts us at a greater risk of suffering a fall. Also, as we become sedentary and weak, the recovery process if an injury does occur is often much slower than it would be for someone who is fit and active.
In the clinic we will look at functional measures including walking, standing on one foot and a sit to stand test to help us determine walking pattern, balance and lower extremity strength. While walking, we want to see that the leg swinging through is lifted high enough to fully clear the ground. A shuffle pattern can result in catching the toe quite easily. As well, since a large portion of walking is spent standing on one foot while the other leg is swinging through, we want to assess balance and stability on the stance leg.
To avoid tripping while walking, it is important to develop a safe walking pattern. The swing through leg should be lifted high enough to properly clear the ground. We also want to see a pattern of striking with the heel and pushing off the big toe with each step. If unsteadiness is noted while standing on one foot, a walking aid such as a cane or walker should probably be used while walking. A physiotherapist can adjust a walking aid and demonstrate how to use it correctly.
A cane or walker is especially important when walking outdoors where there are many obstacles including uneven ground, curbs and other potential tripping hazards. A walking aid should also be kept close to the bed in case it is needed when getting up during the night. A physiotherapist can teach safe and effective exercises to help improve walking pattern and endurance for those who feel weak or unsteady while walking.
It is also very important to stay active and keep moving. Daily physical activity is essential to maintain aerobic endurance, lower extremity strength and balance. It is never too late to start an exercise program. It is important to find an activity that is enjoyable to stay motivated to keep active. This may include walking, hiking, cycling, swimming, golfing, tennis, Tai Chi, yoga or Pilates. In addition to aerobic activity, a physiotherapist can design an appropriate home exercise program to help improve endurance, balance, coordination and strength.
Vestibular Rehabilitation (Dizziness and Vertigo)
Vertigo, Inner Ear & Dizziness
Vestibular Rehabilitation’ is an area of focus in my physiotherapy practise – I am often asked what exactly that means. The vestibular system (involving your inner ear) is responsible for sense of movement, body orientation and balance. The vestibular system (along with our eyes, muscles, and joints) send constant feedback to our brain about our body’s movement and orientation.
Dysfunctions, disorders, trauma or viruses that affect the inner ear can be a potential cause of vertigo, dizziness, decreased balance, tinnitus (ringing in the ears) or a change in hearing. As a vestibular therapist I can assess the potential causes of the mentioned symptoms and provide treatment to help decrease dizziness, vertigo and improve balance.
Dizziness is the umbrella term that refers to a sensation of abnormal, unwanted, movement – a feeling of unsteadiness, lightheaded or feeling ‘off’. Vertigo is a more specific term and implies that there is a rotational component to your dizziness – either the room is spinning around you or you are spinning in the room. Both vertigo and dizziness are symptoms, not a diagnosis, so part of my job is to figure out the possible cause and provide treatment.
One of the most common conditions within the inner ear that I treat is a condition called BPPV – benign paroxysmal positional vertigo. BPPV is caused by a crystal that is free floating within the inner ear. The signs and symptoms are pretty easy to recognize (vertigo brought on when lying flat, rolling in bed, looking up to the ceiling or bending forward). Treatment for BPPV is also quite effective.
It is also important to recognize that not all causes of vertigo or dizziness are associated with problems in the inner ear. Cardiovascular (heart) disorders, thyroid conditions, anxiety, migraines, neck disorders/injuries and neurological conditions are all potential causes.
Robina Palmer is a registered Physiotherapist and co-owner of Sun City Physiotherapy.
Robina is a graduate of University of British Columbia’s School of Rehabilitation Medicine. She has practiced in sports and orthopaedic rehabilitation in various clinical settings throughout the United States and Canada.
Vestibular Rehabilitation (Dizziness and Vertigo)
The winter Olympics in Sochi was filled with scary crashes in nearly every sport. Hearts sank when seeing chances at a medal slip, the pain on the athletes’ faces, and some of the injuries that resulted. We probably all know someone who has, or have ourselves, taken a big spill at the local hill.
But that’s not the only place where falls can occur, especially during this time of year with the fluctuating melt and freeze of roads and walkways. Slips and trips can happen in the community, even in our own homes, for a variety of reasons. Sometimes we can walk away from them with little injury, other than to our pride, but unfortunately sometimes injuries occur. In order to avoid beginning the spring season hurt, it’s good to know what the risk factors to falls are and to address any concerns that may exist.
Some readers may recall a previous article I wrote about vertigo– a condition that makes you feel like you or the world is spinning. This or other conditions of the vestibular system can contribute to feeling dizzy or losing your balance. The vestibular system is partially located in the inner ear, and gives our brain information about where our head is relative to gravity. When it is affected, a conflict of information between the vestibular system and other sensory systems happens. Some related conditions include: Benign Paroxysmal Positional Vertigo (“BPPV”), labryinthitis or neuritis (types of infections), or Ménière’s disease. This in turn may cause vertigo, dizziness, or unsteadiness. Some of the causes of vertigo or dizziness can be treated to help you feel more stable on your feet.
Weaknesses in the legs or trunk, sensory conditions of the feet, or decreased ‘proprioception’ (the information about where a body part is relative to the rest of the body) are other risk factors for falling. Proprioception, balance, and strength can be trained through regular exercise. Tai Chi and Yoga are examples of programs that assist in reducing fall risk. However some people require exercises tailored to their individual abilities and needs. It is important to evaluate whether a particular exercise is safe and appropriate for you. Having an understanding of the exercise and of your own abilities is helpful, but when in doubt, it is helpful to consult a health care provider, or discuss with the instructor.
Risk factors for falling don’t only exist within our bodies, but also in our environment. It’s important to note that while the temperatures have been going above freezing, those cold nights and days can result in a layer of ice. Slowing your pace over these areas, wearing proper footwear, and always being aware of the conditions will help. Within your home, having adequate lighting, keeping the floors and hallways clear of obstacles, and keeping rugs or carpets secured down will also reduce your chances of tripping.
With the example of the Olympic sports of skiing, snowboarding and skating, big falls occur frequently. It’s not often a case of needing to address strength or balance, and rarely is the environment controllable. For these activities, it’s important to protect yourself as much as possible. Wrist guards are light, can fit under gloves, aimed at reducing the risk of a facture when impacting the ground. A common injury with falling is the FOOSH – a ‘Fall Onto an Outstretched Hand’. A brace will keep your wrist in an ideal position and can absorb some of the force to reduce, but not eliminate, the likelihood of a wrist fracture. If you ski, braces also exist to protect the thumb, which can be injured by the ski pole.
If you feel you are at risk of falls, or have an injury after taking one, it is important to see a health care professional to either assist in the prevention of, or in the rehabilitation after, a slip. Reducing the risk can be easy in some situations: adjusting your footwear, modifying your gait aid if you use one (for example, attaching an ice grip onto a cane), making changes to your home environment, or partaking in a strength and balance program designed for your needs. In some cases, dizziness or lightheadedness occurs as a side-effect from medication, so speaking to your doctor may help. From a physiotherapy context, your strength, balance, vestibular function, or any combination of those factors can be assessed and treated as is appropriate for you.

Vestibular Rehabilitation (Dizziness and Vertigo)
It is the weirdest feeling. You get dizzy bending forward or looking up to the ceiling, lying down, getting up in the morning, or even rolling over in bed. It’s like the room is spinning and it makes you feel sick. If you experience this, you may be suffering from Benign Paroxysmal Positional Vertigo (BPPV).
It is estimated that one in every five people will develop vertigo in their lifetime. The most common cause of vertigo is a condition in the inner ear known as Benign Paroxysmal Positional Vertigo. BPPV occurs when there is ‘debris’, or more specifically, a calcium carbonate crystal, which has been displaced within the inner ear. The presence of this displaced crystal within the inner ear can disturb one’s balance and equilibrium, and sense of motion.
These crystals are naturally occurring in the inner ear, attached to a specific structure, and not ‘free floating’. There are multiple causes for the crystals to be displaced but, more often than not, it tends to be spontaneous. Other causes can include trauma (fall, hit to the head, whiplash), high dose antibiotics, age, and extreme changes in barometric pressure.
Most of my patients with BPPV report dizziness with certain positions. Most commonly, it is lying flat in bed, rolling over in bed, getting up in the morning, looking up to the ceiling, and bending forward.
Treatment for BPPV is very effective. It consists of ‘repositioning’ the crystal in the inner ear. This is done through a series of head and body positions, which will move the crystals away from the sensitive hair cells within the inner ear.
Although BPPV accounts for a large percentage of vertigo, it is not the only cause. Talk to your doctor or physiotherapist certified in vestibular rehabilitation if you have these symptoms, or think you may have BPPV.
Robina Palmer is a registered Physiotherapist and co-owner of Sun City Physiotherapy.
Robina is a graduate of University of British Columbia’s School of Rehabilitation Medicine. She has practiced in sports and orthopaedic rehabilitation in various clinical settings throughout the United States and Canada.