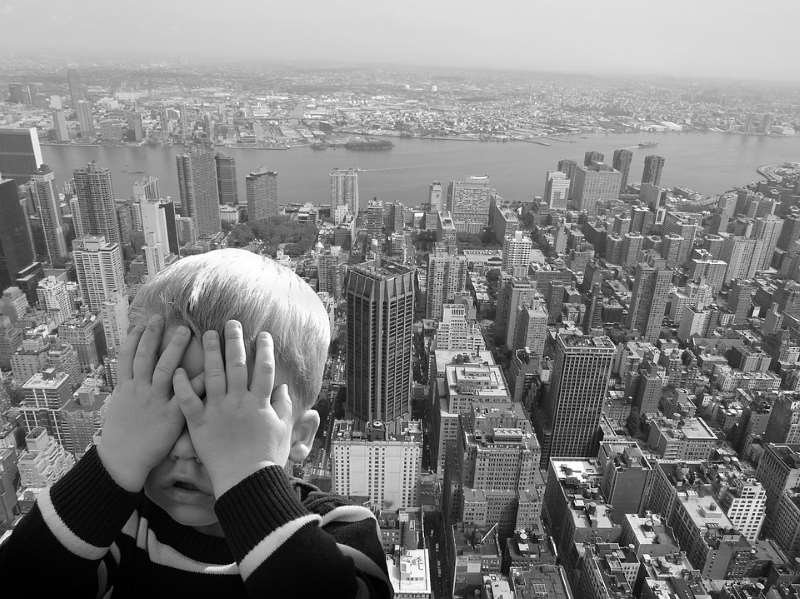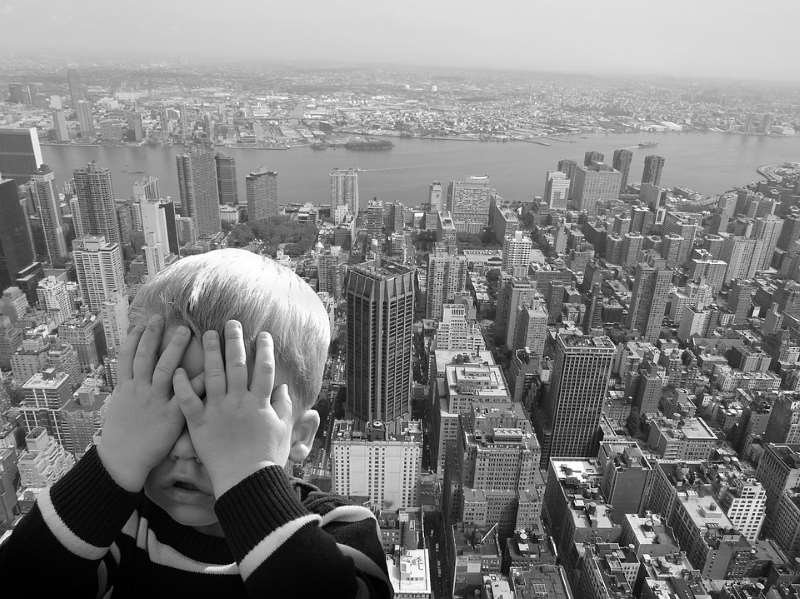
Vestibular Rehabilitation (Dizziness and Vertigo)
Vertigo, Inner Ear & Dizziness
Vestibular Rehabilitation’ is an area of focus in my physiotherapy practise – I am often asked what exactly that means. The vestibular system (involving your inner ear) is responsible for sense of movement, body orientation and balance. The vestibular system (along with our eyes, muscles, and joints) send constant feedback to our brain about our body’s movement and orientation.
Dysfunctions, disorders, trauma or viruses that affect the inner ear can be a potential cause of vertigo, dizziness, decreased balance, tinnitus (ringing in the ears) or a change in hearing. As a vestibular therapist I can assess the potential causes of the mentioned symptoms and provide treatment to help decrease dizziness, vertigo and improve balance.
Dizziness is the umbrella term that refers to a sensation of abnormal, unwanted, movement – a feeling of unsteadiness, lightheaded or feeling ‘off’. Vertigo is a more specific term and implies that there is a rotational component to your dizziness – either the room is spinning around you or you are spinning in the room. Both vertigo and dizziness are symptoms, not a diagnosis, so part of my job is to figure out the possible cause and provide treatment.
One of the most common conditions within the inner ear that I treat is a condition called BPPV – benign paroxysmal positional vertigo. BPPV is caused by a crystal that is free floating within the inner ear. The signs and symptoms are pretty easy to recognize (vertigo brought on when lying flat, rolling in bed, looking up to the ceiling or bending forward). Treatment for BPPV is also quite effective.
It is also important to recognize that not all causes of vertigo or dizziness are associated with problems in the inner ear. Cardiovascular (heart) disorders, thyroid conditions, anxiety, migraines, neck disorders/injuries and neurological conditions are all potential causes.
Hips and Knees, Physio Articles
Hip osteoarthritis is a common condition that involves the degeneration of the articular cartilage of the hip joint. If you have this condition and are noticing an increase in pain and a decrease in physical function you may be wondering what treatment options are available to you.
With osteoarthritis of the hip you may feel a constant ache localized to the groin and side of your hip and sometimes extending into the front of your thigh and knee. The hip often feels stiff, especially first thing in the morning when you get out of bed and it can make activities of daily living much more painful including standing, walking and stairs. It can also make it difficult to put your socks on, get into and out of your car and even get on and off of the toilet.
Stiffness, pain and having difficulty with many previously easy daily activities may lead you to want to do less physical activity. The trouble is, not moving will often lead to weakness, further stiffness and general deconditioning.
A physiotherapist can help design a treatment program with a focus on decreasing pain, increasing range of motion and flexibility, improving core stability, gaining muscle strength and endurance and improving general conditioning. Other functional goals often include improving walking pattern, speed and distance, ability to go up and down stairs without pain and better control going from sit to stand.
This is often accomplished through a combination of education, manual therapy and exercise. An exercise program is often extremely beneficial to help improve physical function and decrease pain. A physiotherapist is an excellent resource to put together a safe and effective home exercise program for you to perform daily at home or at your local gym. Also, if you enjoy swimming, bring this up with your physiotherapist as aquatic exercise is a great form of treatment for hip osteoarthritis.
Other possible physiotherapy treatments that may be effective for some individuals with arthritis of the hip include: acupuncture, massage, heat on the muscles around the hip, ice, TENS, supportive footwear and/or a gait aid such as a cane or walking poles. It is important to talk with your doctor about your arthritis to discuss other treatments that may be beneficial to help manage your symptoms. Certain medications may be helpful, but it is important to bring this up with your doctor to be sure they are appropriate for you. Also, if you are overweight, a weight management program can be extremely beneficial to decrease the stress on your joints. Since nutrition plays a crucial role in weight management, it is important to have this discussion with your doctor.
A small portion of individuals with hip osteoarthritis will eventually opt to have a total hip replacement. This is often the case when symptoms are progressively getting worse and significantly limiting activities of daily living. If you have had a total hip replacement a physiotherapist guided post-operative hip strengthening program is ideal in order to decrease pain, improve your hip function and return to your active lifestyle.
Sports
Running is a popular activity that can help maintain or improve your cardiovascular fitness and in some cases help you lose weight. There are many different reasons to run but often there is a goal set that may include 5Km, 10Km, half marathon, or full marathon.
When training for longer runs including 10km, half and full marathons it is important to remember that the training schedule should take place over long periods of time to allow your muscles and joints to accommodate for the increased strain that will be placed on them during the long run. As a physiotherapist, I treat many runners with all sorts of injuries. Some of the most common injuries include plantar fasciitis, achilles tendonitis, muscle strains, and Iliotibial band friction syndrome (IT band syndrome).
IT band syndrome is a repetitive stress injury that occurs when the iliotibial band glides over the lateral femoral condyle on the outside part of the knee. The iliotibial band is the thick band that runs from the outside of the hip down to the outside of the knee. It is a common injury for long distance runners (20-40 miles/week) but is not limited to only long distance runners. Running on various terrains can increase the risk of developing this condition. Up and down hills, graded slopes, and cambered roads have all been shown to increase the risk. This syndrome may also be found in other athletes or weekend warriors such as cyclists, weight lifters, and participants in jumping sports.
With IT band syndrome there is rarely a history of trauma. Patients will often complain of knee pain that may be difficult to localize and usually increases with repetitive motions like running. The symptoms usually get worse with changes in training surfaces, increasing mileage, or training on crowned roads.
Studies have found that long distance runners with IT band syndrome have weaker hip abductor and glut muscles on the involved leg compared to the uninvolved leg. The hip abductor muscles are located on the outside part of the hip and help prevent the leg from moving towards the centre of the body. It is also noted that fatigued runners are more prone to having their hip adduct (move towards the centre) and internally rotate (leg turns inwards) which causes more friction on the iliotibial band and therefore the symptoms get worse.
The management of IT band syndrome usually includes: 1) activity modification (usually decreasing mileage). 2) New running shoes. Shoes should be replaced about every 500km. 3) Heat or ice. 4) Stretching the IT band. 5) Strengthening the hip abductors and glut muscles.
If you are interested in pursuing long distance running you should: 1) follow a certified training schedule. 2) Make sure the shoes you are wearing are the right shoes for you. 3) Increase your mileage slowly to allow your body to accommodate for the increased strain. 4) Hit the gym – muscle weakness can cause problems down the road. 5) Go in for an assessment with a health care professional if you start to experience aches and pains that aren’t going away.
TMJ / Jaw
Did you wake up this morning with acute facial pain and inability to open your mouth? When you think to yesterday, you remember taking a big bite from an apple and experienced a sharp pain in your jaw joint. Today, you can’t really open or fully close your mouth. That unexplained clicking in your jaw that you’ve had for two years has suddenly gone away. Now, there’s just facial tenderness in front of your ear and you’re worried that you can’t eat! If you experience this, you likely have a “locked jaw”, or Acute Disc Displacement. This is one of the common disorders of the Temporomandibular Joint, more known as the TMJ.
The TMJ is the ball and socket joint that connects the Mandible (jaw bone) and the Temporal bone (one of the bones of your skull). It’s the small joint located in front of your ear. There is a cartilage cushion in between the ball and socket, referred to as the Disc. The disc is supported by special Ligaments, which keep the disc in place. Movement problems of the disc can be responsible for creating many symptoms in the TMJ, such as clicking, crepitations, locking, muscle spasm, and pain.
TMJ Disorder/Dysfunction, or TMJD/TMD, is seen more commonly in women than men. There is a 3:1 incidence in females to males, and can include one or both jaw joints. In most instances, the dysfunction is a result of an imbalance or change in the normal function of the bones, ligaments, muscles, disc, or nerve components of the TMJ complex.
Disc Displacement is a mechanical problem that occurs when the disc ends up in the wrong position within the ball and socket. In this case, it is likely that the disc has become displaced due to the wide opening, creating increased stress and strain on the ligaments, resulting in pain around the joint and spasm in the facial muscles. There is also a longstanding history of unexplained clicking in the joint, which may be a pre-disposing factor to this problem. In essence, the disc needs to be properly re-educated to find its’ normal resting position again, and the mechanics restored to the muscles and joint. Specialized physical therapy care would assist in restoration of disc position, to restore movement and function, as well as normalize the pain.
Dysfunction in these tiny joints can have many causes. These can include trauma such as blow to the head, whiplash, falls, sports injuries, arthritis, dental occlusion, dentures, history of joint noises, stress (clenching, grinding), poor habits (posture, physical, oral), and many others. Signs and symptoms may include facial pain, headache, neck pain, ear pain, sudden changes in bite, tooth pain, ringing in the ears, shoulder pain, and facial tingling or numbness.
A physical therapist can help you understand and manage your TMJ dysfunction. Often it is obvious that the TMJ is the cause of symptoms you experience. However, for many people, the symptoms they experience can be widespread, and may not make it so obvious. As mechanics for the human body, physical therapists can properly assess, diagnose, and treat the TMJ and most of the possible influences. We provide a specialized hands-on approach to treatment, education, and exercise program. Treatment may also include other muscle re-education techniques such as Intramuscular Stimulation (IMS). In many instances, we often work with your oral practitioner (dentist, orthodontist, oral surgeon) to ensure the best outcome possible for your TMJ. Treatment can be very effective in a short period of time. A self-applied approach with a little guidance from specialized physical therapy practitioners will help with long-term benefits.
Acute Disc Displacement is only one of several diagnoses of TMJ dysfunction. Keep connected to read about other problems that these tiny joints can give you. Don’t stop eating apples though…
Elbow, Wrist and Hand
Tennis Elbow – you don’t need to play tennis to get it!
Tennis elbow is so called as one of the reasons you can get it is from faulty technique in a tennis shot. This is only one of the ways that you can get tennis elbow though, it can come on from many other activities that involve a lot of wrist and forearm use.
The medical name for this condition, lateral epicondylitis, gives us more information about where the problem occurs. The lateral epicondyle is a small bony prominence on the outside of the elbow and is the point of attachment for the tendons of the wrist extensor muscles. These muscles run up the top of the forearm and play a role in movements such as bending the wrist back, making a fist, and twisting the forearm.
Lateral epicondylitis occurs if these muscles are used more than they are used to, resulting in pain and damage to the tendon where it attaches onto the bone at the lateral epicondyle. If you have tennis elbow, you will likely report an increase in pain when gripping tightly or shaking hands, using a screwdriver or twisting a jar, or any activity that requires wrist and hand use. The outside of the elbow can be very sensitive to touch, and you may find it will get very stiff, especially first thing in the morning.
In order to treat tennis elbow, it is important to identify the reason why it became injured in the first place and correct that. Apart from stopping the aggravating activity, there are often other contributing factors that need to be changed in each individual case. These can be related to our own anatomy in the elbow and arm, movement patterns which are overloading and therefore damaging the tendon, or factors relating to the equipment being used.
A physiotherapist can identify the changes that need to be made in each individual case and implement these. As well as this there is specific treatment that can be done to the tendon to ensure optimal healing such as friction massage and laser, and a stretching and strengthening program should be implemented too to ensure the muscles and tendons are in good shape to be able to cope comfortably with being used in the future.
So even if you don’t play tennis, you can still be affected by tennis elbow. Taking the right action will take your pain away.